Dermatologists perform Skin Cancer Check at a specialist level. We apply clinical, dermatoscopic & photographic methods to map & follow up lesions of concern. Early detection of skin cancer confers a higher survival rate.
Key Points
- Australia has the highest incidence of melanoma in the world
- Queensland has the highest incidence of melanoma in Australia
- Moles will increase in size & number until your mid 30s
- A sudden change in shape, colour, border, or size may point toward malignant change
- Early detection of melanoma increases survival rate
Skin Cancer Check at a glance
Our results speak for themselves

Before
After
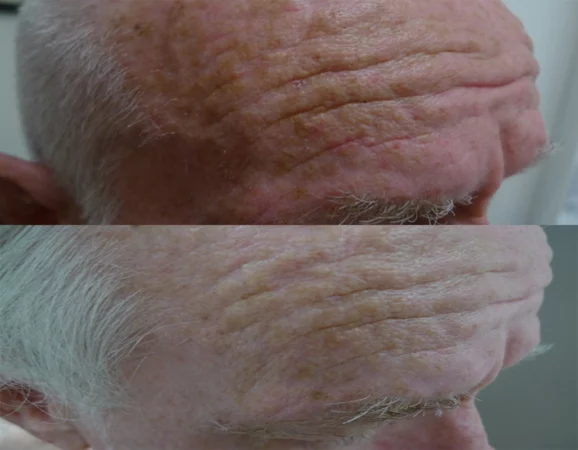
Excision + 1927 thulium overpass to
adjacent solar keratosis
Ask us more about this treatmant
Preferred Consultation

Before
After

Photodynamic Therapy, thulium assisted
for solar keratosis. PDT is covered under
DVA
Ask us more about this treatmant
Preferred Consultation

Before
After

Thulium HD, 1927 overpass. 1 session, 5
day recovery
Ask us more about this treatmant
Preferred Consultation
FAQs
How common is melanoma in Queensland?
Australia has the highest rates of melanoma in the world. 1 in 14 males and 1 in 22 females will develop invasive melanoma in their lifetime (to age 85).
The earlier a cancer is detected, the higher the chances of survival.
What is the difference between a dermatologist & skin cancer doctor?
5 years of formal education. Dermatologists are specialists in skin cancer management, this means we all undergo structured training in public hospitals. Training includes management of high-risk patients including-
- High risk melanoma detection & research
- Immunosuppression organ transplant patients
- Joint dermatology, plastics & radiation oncology clinics
- Management of all types of skin cancer
Dermatologists at Cutis hold hospital positions at Greenslopes, Queensland Institute of Dermatology, the Royal Brisbane Hospital, Mater adults & Queensland Children Hospitals.
How does training translate to skin checks?
We handle every case of skin cancer management, from simple mole checks, through to difficult complex presentations including moles in babies, high risk patients & rare skin tumours.
We also use the very latest technology including lasers to address pre-cancerous lesions & employ photographic systems to detect early changes in moles.
What types of moles are there?
Moles are by definition, benign (noncancerous) growths. They occur in babies, children & adults. The classification is complex. Most moles have an extremely low chance of turning into skin cancer. A simple classification is-
- Junctional & compound naevi- most common moles
- Intradermal naevi- presents as skin-coloured moles
- Dysplastic moles- abnormal moles with a potential for malignant change
- Congenital melanocytic nevus- moles since birth
- Blue nevus- deep blue moles, frequently confused with melanoma
- Collision naevi- characteristics of two or more skin lesions
What are my risks of cancer if I have a lot of moles?
It’s all about numbers, probability & genetics.
A large number of moles can act as a marker for developing melanoma at each mole has a chance of malignant change. Other factors that come into play include-
- Race & ethnicity. Fair skin types have increased incidence of skin cancer
- Genetics: a family history of skin cancer increases your odds of developing both melanoma & non-melanoma skin cancer.
- Sun exposure & UV radiation, including sunburn increases the odds.
- Immune suppression increases both melanoma & NMSC rate.
How to keep track of moles?
If you have lots of moles, especially odd-looking moles, it may not be possible to excise all of them. Dermatologists will weigh up factors including clinical history, family history, as well as dermatoscopic & clinical finding of each mole. From there, we-
- Take note of the findings & arrange a future review to monitor stability.
- Take photos of high-risk moles then review.
- Organise serial photographic scanning then review.
- Excise for pathology testing.
What is the ABCD rule of mole surveillance?
The ABCD rule is a guide to early detection of melanoma based upon probability & not possibility. It stands for-
- Asymmetry – the mirror image of one half is different from the other.
- Border changes – the edges are often ragged or irregular in outline; the pigment may spread into the surrounding skin, blurring the outline of the mole.
- Colour – the colour is uneven, consisting of many shades of black, brown, & possibly even red, pink & blue.
- Diameter – increase in the size of the mole, with a diameter of 6 mm or more.
This rule will not pick out every single melanoma, however 90% of cases follow this pattern.
Our dermatologists are experts in skin checks. We manage all risk profiles– from simple lesion checks to complex high risk patients.
What is the EFG rule?
The EFG rule is another guide that recognizes a subtype of melanoma that can grow quickly. It stands for-
- Elevated — moles that are raised on the skin.
- Firm — moles that are firm to touch.
- Growing — moles that grow and change very rapidly.
Why do self-checks & what is the value?
It is all about increasing the odds for early pick up & survival. The scientific data points out that up to 40% of melanoma cases are detected at home, during a self-examination. Survival rate is proportional to how early cancers are diagnosed.
Following the ABCD EFG rule increases sensitivity, especially if you take photos of moles yourself. Self-checks are augmented by a real time visit to a dermatologist every 3 to 6 months.
High risk patients including a previous history of melanoma, family history or a history of multiple dysplastic moles have the option for another layer of surveillance, namely state of the art photographic documentation, namely Mole Mapping.
What are other characteristics to look for when performing a skin check?
Melanoma doesn’t always fit the ABCDE or EFG rules. Other helpful features include-
- A mole that is different from others.
- Changes in shape, coloration & size.
- Symptoms including itch.
- A new spot or mole
- A lesion that bleeds
If you have a lesion of concern, ask your GP to refer you to a dermatologist for an urgent review.
What types of moles occur in children & what is the risk?
Dermatologists are involved in high risk, hard calls. This is one of them. There are
two types of moles occurring in children that can be alarming.
Congenital melanocytic naevi: a dark mole present from birth. They can be classified as small, medium, or large. Malignant changes are mostly seen in large lesions, with the odds ranging from 1-3%, lifetime risk.
Spitz naevus. This can be tricky; the management goes beyond the scope of this page.
For mole checks in babies & children, Cutis has a team of paediatric dermatologists. Reception will guide you through the referral process. Our team also consults at the Queensland Children’s Hospital, department of dermatology.
Do we provide cosmetic mole removal?
It depends on the site & clinical scenario. To mitigate the risks of scarring, we perform a shave excision. This has pros & cons.
Pros: Less chances of scarring, lesion submitted for testing to exclude cancer.
Cons: Higher chance of recurrence.
We do not laser moles, due to the chances of pseudo-melanoma. Google this, & you can see why we don’t apply laser light to moles.
What is Mole Mapping & when do we use it?
Mole mapping is useful to keep track of lots of moles. This can –
- Pick up early changes
- Reduce the requirement for excisions
- Keep a record of your moles
Mapping uses specialised cameras that cover your entire body. The moles are then read, then followed up for changes. This is a useful service if you have lots of mole & or at higher risk of developing melanoma. It is invaluable in the management of familial dysplastic moles.
MoleMap’s clinical excellence is the gold standard for the detection and diagnosis of melanoma & non-melanoma skin cancer.
Do you require a mole check if you have ethnic skin?
In this case it is about possibility & not a probability. If you are of Asian, Islander, or African descent, the chances of melanoma are very slim. Most melanomas in these races occur on the palms, soles, nail beds & unusual areas such as the eye & mucous membranes.
Based purely on statistics, you are unlikely to develop melanoma in your lifetime, however, if your mole follows the ABCDEFG rule, it is prudent to get a skin check to rule out cancer.